
Perhaps of most concern is that despite more than a century of infection prevention that has paralleled many advances in IV therapy, there is a dearth of evidence supporting which specific aseptic technique provides the most effective prevention against the risk of infection. Moreover, given the incidence of particularly high-profile organisms such as MRSA, IV therapy has consistently been identified as a particularly problematic area for aseptic technique. However, despite this, historically and contemporaneously, the field of IV therapy fairs no better in aseptic technique than any other field of clinical practice. Given the significantly invasive nature of inserting indwelling medical devices and their ongoing care and maintenance, aseptic technique has always been of much concern in the field of intravenous therapy.
2007), Saving Lives (DH 2007) and the 100,000 Lives Campaign (Berwick et al. 2006 Pronovost 2008), 5 Moments for Hand Hygiene (Sax et al. As a result, concern for standards of aseptic technique has been reflected in a wide range of international initiatives concerned with improving infection prevention such as the Keystone project (Pronovost et al. But most concerning of all is the effect of a confused literature on clinical practice with poor standards of aseptic technique commonly and consistently reported (Hartley 2005 Flores 2008 Aziz 2009 Rowley et al. In education, students and qualified staff are taught various educational concepts and practical methods of performing essentially the same activity using different methods and descriptors (Hartley 2005 Flores 2008 Aziz 2009 Rowley et al. Such ‘prescription without explanation’ by major stakeholders appears to have undermined this critical clinical competency and potentially fuels the complacency associated with aseptic technique. Internationally, it seems to have become ‘fashionable’ for guideline makers to address the historical confusion surrounding aseptic technique by simply prescribing the generic term ‘aseptic technique’, with virtually no meaningful explanation of what aseptic technique is or how it is to be applied to ensure patient safety (NICE 2012 Gorski et al. Historical and contemporary literature presents a confused hierarchy of terms and practices including sterile technique, aseptic technique, clean technique and non-touch technique, further compounded by interchangeable use and meaning (Aziz 2009 Rowley et al. Although the prescription for aseptic technique is universal, agreement on the aim, definition, description and application of aseptic technique is not (Preston 2005 NICE 2012 Gorski et al. In terms of protecting patients from infection, aseptic technique is one of the most important and commonly used critical clinical competencies in healthcare.

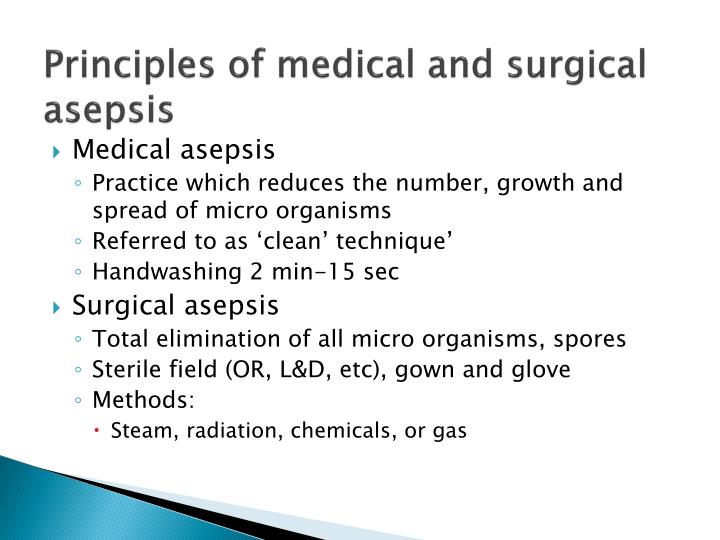
A combination of decontamination processes, sterilized equipment and handling technique is used to minimize potential transmission of pathogenic microorganisms (Clare and Rowley 2017). KeywordsĪt its heart, aseptic technique involves a collection of infection prevention actions designed to protect patients from infection when undergoing invasive clinical procedures, including maintenance of indwelling medical devices.

EXAMPLE OF MEDICAL ASEPSIS HOW TO
This chapter provides clinical examples of how the ANTT ® is implemented in the healthcare setting, as well as, importantly, how to promote compliance of the technique. During the insertion or manipulation of an intravascular device, the ‘ANTT-Approach’ provides a systematic method that supports the practitioner to include all the important elements of aseptic technique, with particular focus on the identification and protection of ‘Key-Parts’ and ‘Key-Sites’ throughout the preparation and the procedure. The ANTT ® Clinical Practice Framework provides a comprehensive framework for aseptic technique for all invasive procedures based on an approach termed Key-Part and Key-Site Protection. The Aseptic Non Touch Technique (ANTT ®), originated by Rowley in the late 1990s, was designed to help address variable aseptic technique standards of practice and provide a rationalized, contemporary, evidence-based framework to standardize this critical competency and help improve standards of practice. However, no meaningful explanation of what aseptic technique is or how it is to be applied to ensure patient safety is provided within any of the guidelines. Aseptic technique, which involves infection prevention actions designed to protect patients from infection when undergoing invasive clinical procedures, is universally prescribed by guideline makers as a critical competency in the prevention of infections.


 0 kommentar(er)
0 kommentar(er)
